
This is called a transfusion reaction, and it occurs immediately when incompatible blood is transfused. If you get a transfusion that has different antigens (incompatible blood), the antibodies in your plasma will destroy the donor blood cells. have type AB blood, with 1% having AB-negative (AB-) blood and 4% having AB-positive (AB+) blood.īlood received in a transfusion must have the same antigens as yours (compatible blood). About 5% of people (5 in 100) in the U.S.
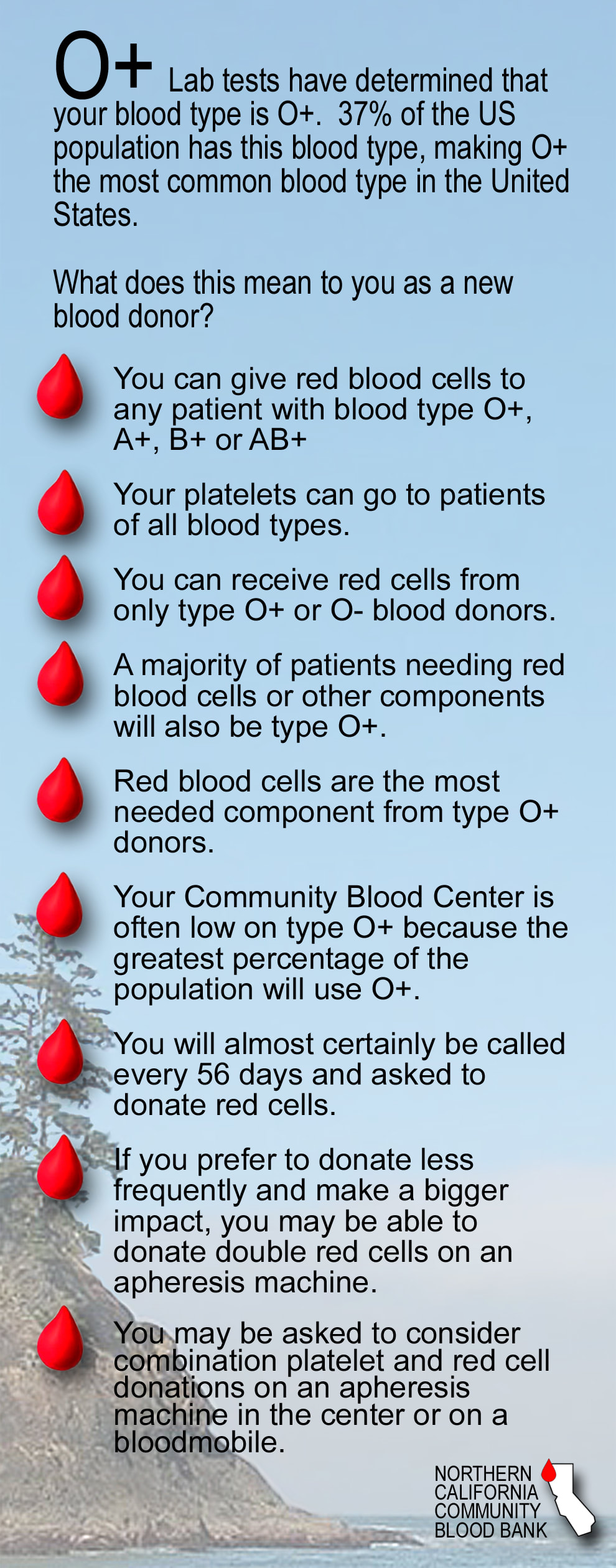
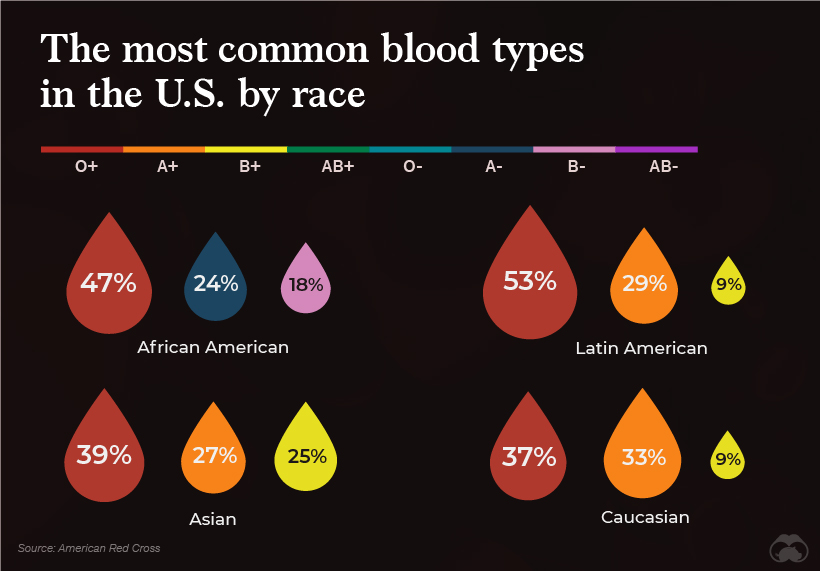
Your plasma does not have antibodies against type A or type B blood. have type O blood, with 9% having O-negative (O-) blood and 39% having O-positive (O+) blood. About 48% of people (48 in 100) in the U.S. Your plasma has antibodies that attack both type A and type B blood. have type B blood, with 2% having B-negative (B-) blood and 9% having B-positive (B+) blood. About 11% of people (11 in 100) in the U.S. Your plasma has antibodies that attack type A blood. About 36% of people (36 in 100) in the United States have type A blood, with 6% having A-negative (A-) blood and 30% having A-positive (A+) blood. The liquid portion of your blood (plasma) has antibodies that attack type B blood. If your red blood cells have: The A antigen. The ABO test shows that people have one of four blood types: A, B, AB, or O. So the two most common blood type tests are the ABO and Rh tests. The most important antigens are blood group antigens (ABO) and the Rh antigen, which is either present (positive, +) or absent (negative, -). Blood type tests may also be done to see if two people are likely to be blood relatives. Human blood is typed by certain markers (called antigens) on the surface of red blood cells. We also offer antenatal courses which are a great way to find out more about birth, labour and life with a new baby.Blood type tests are done before a person gets a blood transfusion and to check a pregnant woman's blood type. Our support line offers practical and emotional support with feeding your baby and general enquiries for parents, members and volunteers: 03. These treatments might include phototherapy (light therapy), sometimes intravenous antibodies from healthy donors and rarely a blood transfusion (NHS, 2018). Others may be need to be born early so that they can have treatments. Rarely, the baby may need a blood transfusion while they’re in the womb (NHS, 2018). Babies with rhesus disease: treatmentĪround half of all cases of rhesus disease need barely any treatment, with the baby simply being monitored regularly during pregnancy (NHS, 2018). If it is, and you aren’t immune, you’ll be offered another anti-D injection (NHS, 2018).
It’s up to you if you want to take the injections though.Īfter the baby has been born, their blood will be checked to see whether it is RhD-positive. You can have anti-D either as a one-off dose at 28 to 30 weeks or as two doses at 28 and 34 weeks (NHS, 2018).Īnti-D is a blood product that can mop up rhesus positive antigens (NHS, 2018). While the evidence about the benefits of this approach isn’t conclusive, NICE recommends routine anti-D injections for all pregnant RhD-negative women in case sensitisation occurs (NICE, 2008 McBain et al, 2015). If you’re rhesus negative and your partner is rhesus positive, you might be offered a couple of extra midwife appointments for ‘anti-D’ injections. Unfortunately, there’s no standard way of knowing whether your baby is rhesus-positive as testing is expensive and doesn’t happen as standard in the UK (Hawk et al, 2013). That can result in anaemia and jaundice in the baby (NHS, 2018). If that happens, the baby may get rhesus disease or haemolytic disease of the foetus and newborn (HDFN). It might also happen after a previous miscarriage or ectopic pregnancy, or very rarely during a blood transfusion (NHS, 2018). Your baby’s blood can transfer to you during birth, or if you have a bleed, an injury like a fall or a car accident, or an invasive medical procedure (NHS, 2018). The danger of that is that your immune system can develop antibodies against it that then attack the baby’s red blood cells. If you are rhesus negative but have a rhesus positive baby, the baby’s blood can enter your bloodstream. But if you have more babies, you might need extra care. And that’s where things get a bit complicated… Rhesus negative: issues for the babyīeing rhesus negative is not a problem in your first pregnancy. In about 10% of all births in England and Wales, the mum is RhD-negative and the baby has inherited RhD-positive blood from the dad (NICE, 2008). The blood test will also show if you’re rhesus positive (RhD-positive) or rhesus negative (RhD-negative).Ībout 15% of the UK population are rhesus negative and 17% of all births in England and Wales are to rhesus negative women (NICE, 2008). You’ll have a test for your blood group (A, B, AB or O) in your initial booking in appointment.


 0 kommentar(er)
0 kommentar(er)
